 Ilustrasi (Atlascompany/Freepik)
Ilustrasi (Atlascompany/Freepik)
The Earlier, the Better
The 90-90-90 narrative on HIV treatment states that 90% of all people living with HIV will know their HIV status, 90% of all people with diagnosed HIV infection will receive sustained antiretroviral therapy, and 90% of all people receiving antiretroviral therapy will have viral suppression by 2020. Regardless of the newly ambitious and final narrative, Indonesia still reports new high cases of HIV per year and the cascade of HIV testing and treatment uptake is low. There is an urgent need to find the most suitable intervention to improve the treatment cascade.
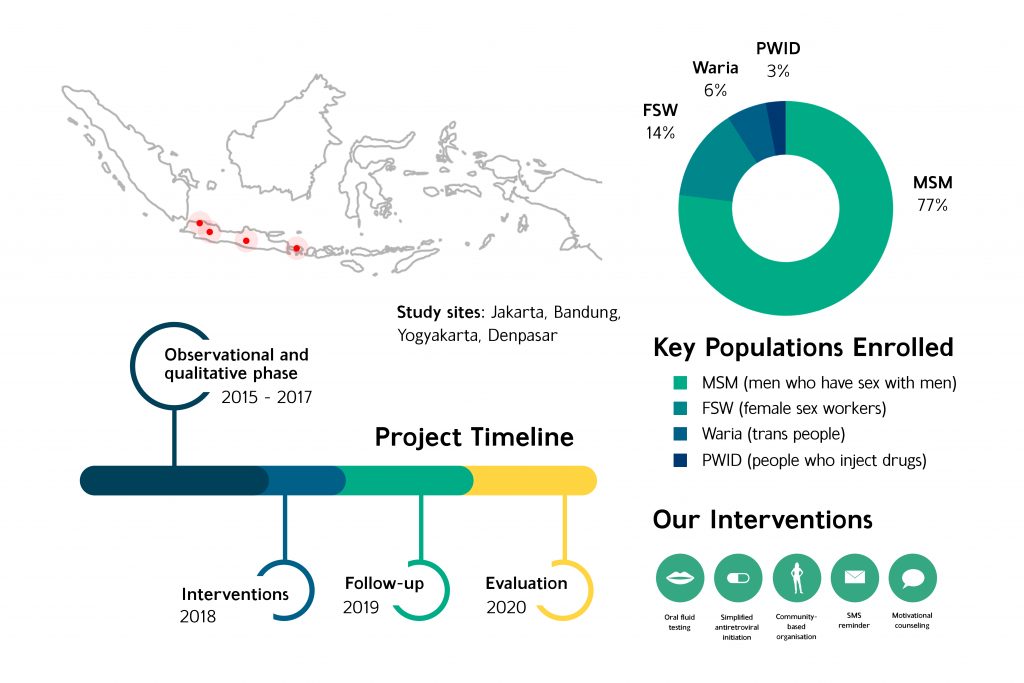
Study on HIV Awal (Early) Test and Treat Indonesia–known as HATI Study–was a collaborative initiative between research centers, government, NGOs and stakeholders that seek for solutions regarding the HIV management in Indonesia. The research was conducted in 2015 – 2020 and took place in multiple cities like Jakarta, Bandung, Yogyakarta, and Denpasar.
The observational and qualitative phase evaluated prior-to-current situations of HIV care and its key populations, and from that we tried to establish new solutions on the next interventional phase. Study participants were predominantly men who have sex with men and female sex workers, followed by transgenders (waria) and people who inject drugs. Based on the first phase of study, it was agreed that numerous novel interventions should be implemented according to three main goals: to increase testing, to increase antiretroviral (ARV) initiation, and to ensure retention of those who started treatment.
Oral Fluid Testing
One of the interventions aims to cover MSM-targeted screening by oral fluid testing (OFT) in Denpasar. HATI distributed OFT in January-December 2018 to 813 MSM in Bali, among 813 participants, 93% chose supervised testing and 7% unsupervised. The OFT result was reactive for 83 participants, of whom 52 out of those 83 underwent confirmatory testing with 47 out of 52 found to be HIV positive. Among confirmed positives, they were enrolled in HATI study cohort and started treatment. At six months follow up, 64% of those initiating treatment were still receiving it, and all had a suppressed viral load. There was an increase in the mean number of MSM tested for HIV by HATI study Bali sites per month, these findings show the potential utility of offering HIV oral fluid self-test kits to scale-up HIV testing in MSM key population.
Simplified Antiretroviral Initiation (SAI) Cascade
This study also tried to simplify ARV initiation so that newly diagnosed patients were able to receive fixed-dose-combination regimen upon knowing their status. SAI model is proved to be feasible and able to increase uptake of antiretroviral therapy initiation after HIV diagnosis. The SAI model can be applied in multiple centers like primary care, clinic, and hospital settings. This was shown to be beneficial in centers that had not been equipped with sufficient lab facilities and thus ARV coverage improved.
Community Screening in Pasar Kembang Brothels Area
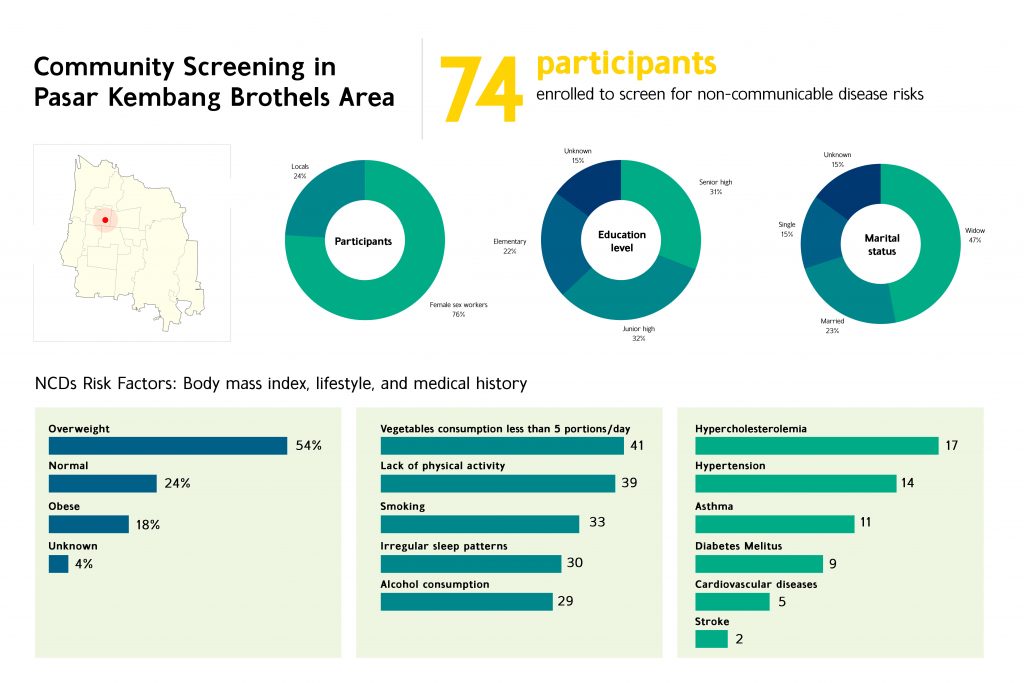
Primary health care services join in collaboration with NGOs like Vesta and Kebaya and Pasar Kembang brothels in Yogyakarta to further their outreach with community-based intervention in which the HIV testing and antiretroviral initiation were conducted simultaneously at community level. This improved coverage and even raised awareness among the general population on knowing their HIV status. Likewise this intervention proved to shorten the testing and treatment time gap significantly.
The sex workers community of Pasar Kembang were trained on the risk and screening of non-communicable diseases alongside with the HIV and other STIs testing. No participants were HIV diagnosed during the services; but most participants were screened positive for non-communicable disease risks like unhealthy diet, smoking, alcohol consumption, and lack of physical activity. From this intervention we know that sex workers community, who has always been framed in the stereotypical society’s view of ‘dirty’ because sexually transmitted infection, also suffers other health problems from non-communicable disease aspect just like everyone of us. Reduced stigma came along with providing integrated non-communicable disease services to HIV service, this was an encouragement for the community to check for their health voluntarily through their fellow trained peers in the future to come.
Short Message Service (SMS) Reminder
This study aims to improve and preserve adherence in those who has started the course of antiretroviral treatment. Upon intervention, this study felt that it was challenging to improve adherence by conducting SMS reminder only. In spite of challenges, SMS reminder has the potential to provide better health access for patients through an integrated health system, especially among pharmacies, patients registry system, and medical record.
Motivational Interview
The motivational interview aims to increase the cascade of ARV initiation and adherence particularly on people who inject drugs, this intervention took place in primary health care services and hospitals in Jakarta and Bandung. There was a slight increase in the participants’ commitment to their treatment adherence. In our opinion, the role of professional counselors and psychologists may be critical in ensuring treatment adherence for people who inject drugs through counseling.
Published works
Januraga, P., Reekie, J., Mulyani, T., Lestari, B., Iskandar, S., Wisaksana, R., Kusmayanti, N., Subronto, Y., Widyanthini, D., Wirawan, D., Wongso, L., Sudewo, A., Sukmaningrum, E., Nisa, T., Prabowo, B., Law, M., Cooper, D. and Kaldor, J., 2018. The cascade of HIV care among key populations in Indonesia: a prospective cohort study. The Lancet HIV, 5(10), pp.e560-e568.
Lazuardi, E., Newman, C., Anintya, I., Rowe, E., Wirawan, D., Wisaksana, R., Subronto, Y., Kusmayanti, N., Iskandar, S., Kaldor, J. and Bell, S., 2019. Increasing HIV treatment access, uptake and use among men who have sex with men in urban Indonesia: evidence from a qualitative study in three cities. Health Policy and Planning,.
Lazuardi, E., Newman, C., Tasya, I., Rowe, E., Wirawan, D., Wisaksana, R., Subronto, Y., Kaldor, J., Kusmayanti, N., Iskandar, S. and Bell, S., 2019. Understanding the Social Influences on Engaging Key Populations With HIV Prevention: A Qualitative Study With Men Who Have Sex With Men in Three Indonesian Cities. AIDS Education and Prevention, 31(3), pp.206-223.
Mitchell, E., Lazuardi, E., Rowe, E., Anintya, I., Wirawan, D., Wisaksana, R., Subronto, Y., Prameswari, H., Kaldor, J. and Bell, S., 2019. Barriers and Enablers to HIV Care Among Waria (Transgender Women) in Indonesia: A Qualitative Study. AIDS Education and Prevention, 31(6), pp.538-552.
Widyanthini, D., Januraga, P., Wisaksana, R., Subronto, Y., Sukmaningrum, E., Kusmayanti, N., Dewi, H., Law, M., Kaldor, J. and Wirawan, D., 2021. HIV self-testing for men who have sex with men: an implementation trial in Indonesia. AIDS Care, pp.1-8.
